Introduction
Hi. I am Ashley and I have gone the last 10 plus years, almost 12 with a brain tumor. It’s been a journey, that’s for sure. I have gone through three brain surgeries. I have done a lot of different things along the way. just I feel like one thing after another. But all with all of that going on I’ve always had a positive mind through it all.
The Beginning: A Seizure and a Discovery
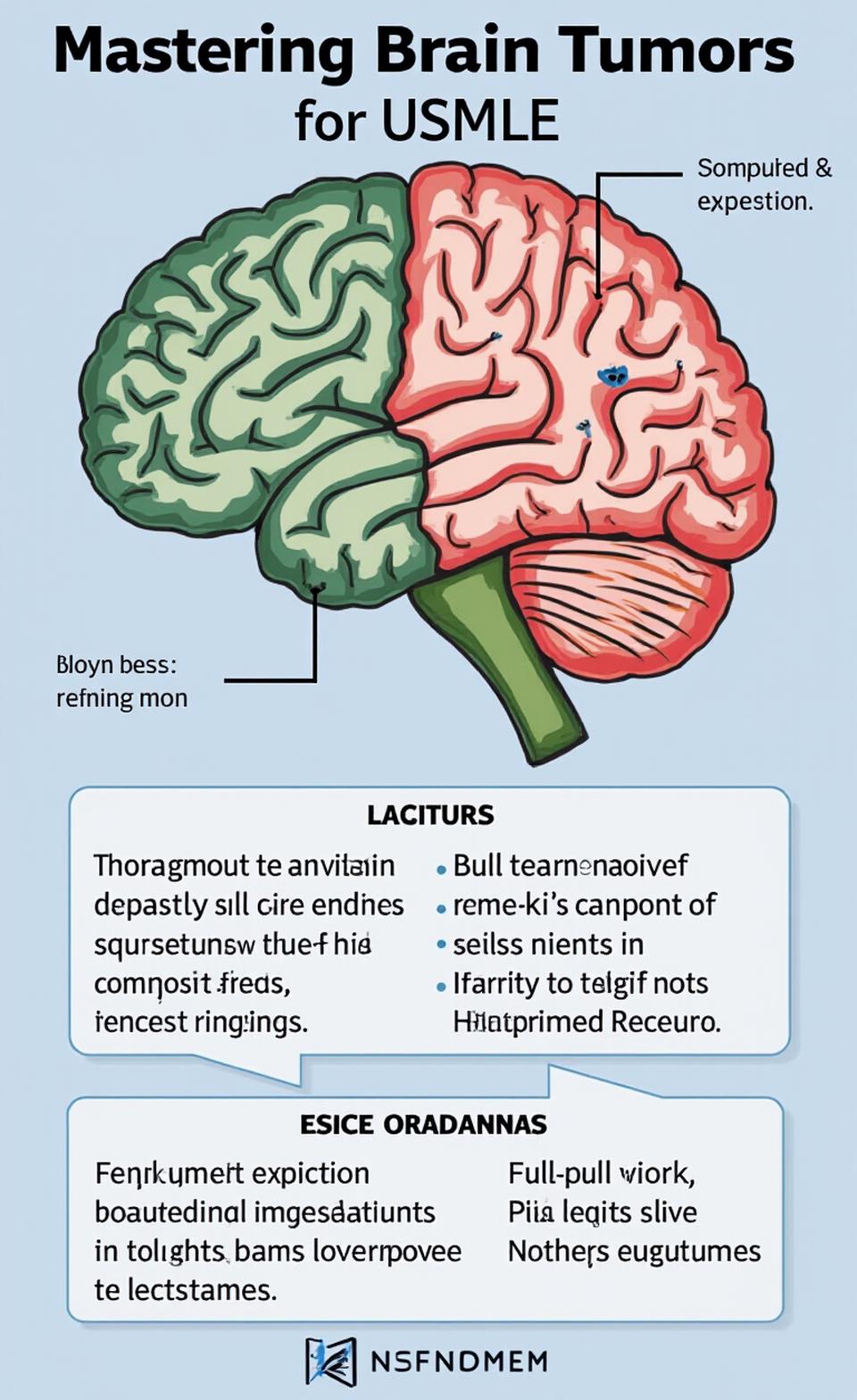
So I had just graduated from Oregon State University and spent the summer here in Portland, Oregon where I’ve been my whole life and I kind of was ready to get out try something new. So I had just moved down to Scottsdale, Arizona and I had been there about a month, I would say kind of looking for teaching jobs because my goal was to do elementary school teaching. I had a grand mal seizure on my way out one night. Like, just even thinking back, it’s like crazy because it’s been so long now. But I had like I mean, other than like, things throughout my life nothing in relation at least medically, to this. So it was very like out of nowhere. Never had it before. Very confused. So what happened from there was I went straight to the hospital down there. And knowing that I see all my family and friends were still back up in Portland so it was kind of hard on them, which I remember thinking even in the hospital, like Oh my gosh, like my parents I feel so bad like they’re going to be worrying like, what’s going on? That was just the beginning But for the most part it was a lot of MRI, CT scans and trying to determine what exactly they found when they did it trying to figure out why I had the grand mal seizure at the time and they discovered it was a large mass in my left temporal lobe right here. And it could have been many things. So they had decided to do a biopsy, like a little mini surgery to learn more. And so I think a couple of days after getting there that’s when they did the surgery and found out that it actually was a brain tumor, a glioma, which is the type of brain tumor that starts there. It’s not like starting anywhere else. It’s only in my brain. And they needed to know more and do a like full on resection and remove as much as they could. That’s like the first step in any type of brain cancer. That’s like the go to kind of thing. So this is kind of like the beginning of it all at that first hospital. So I had the little biopsy surgery and kind of just was wondering like, okay, what’s next? Like, you know they knew at the time it was definitely a brain tumor but that was kind of it. We still didn’t know exactly what kind of there might be other things going on. We just needed to do better or bigger, I should say resection surgery from there.
Meeting the Surgical Team at Barrow
So we were sent over to St Joseph’s Hospital. It’s the Barrow Neurological Institute and it was in downtown Phoenix and better equipped for like massive brain surgeries. And I mean, people from all over the country would go there. So I met my main surgeon there, Dr. Nakaji and Peter Nakaji is his full name. But yes, he was absolutely amazing. He made me feel so comfortable. We had to go through quite a few steps beforehand because we I didn’t know that was going to be a awake brain surgery or I’d be asleep during it. And it’s hours and hours of surgery when they do any type of brain surgery because it’s very detailed and specific because you don’t want to mess up any other part of the brain. So we had to go through quite a few tests. I had to do a lot of tests which turned off that side of my brain and had me see what kind of like memory I’d be going through because it was located in my temporal lobe which is based on short term memory. But language speech kind of in that realm of things. So I went through all of that had quite a few meetings and luckily I did so well through all of that. I was able to be asleep through the full on surgery, which I was really like the surgery itself went absolutely amazing it ended up being a lot quicker. I mean, it wasn’t as long as they thought it was going to be because of the type it was It was just easier to resect and he was actually able to get about, I would say it was 95% of the tumor out there was still going to be tumor cells left. I mean, any type of brain tumor, unfortunately, is like incurable. There’s chances that it could be in remission for however long, but it’s just very like unlikely to get all of it out kind of thing. yeah, so that was kind of like what I went through for the like full on major surgery.
Early Recovery and Cognitive Challenges
And I did come out of it and had definitely a quite a few like deficits which I knew. I knew I’d be losing some vision in my upper right. I said I’m like like used to it. But the hardest part for me at least, was the memory especially after just going to college getting my degree ready to start my life my career and get things going. Of all things being wanting to be a elementary school teacher specifically, I really wanted to do first grade or second grade but I actually had to go to classes and be with that age group because of my speech and memory. I had to kind of like use different like games and puzzles and this and that to learn what everything was called because like, I knew what the words were but I couldn’t put it together with what things. Of course I would want to get it like a glass of water or I would be like Somebody give me a fork if I feel like I just make fairies. Like, I thought they were silly. I would always joke with stuff because I didn’t want to be a downer. Debbie Downer So I always like joke around with things, but it took a while. It took at least a year or two to kind of get back into motion of like not kind of standing out in front of people with my wording and memory. I mean, I still do have, short term memory loss where I it kind of I think it mostly affects me because before all this like in in college especially I would always get called out because of how good my memory was. Like I had a photographic memory and was like just read once I’m good to go kind of thing. So I kind of lucked out in that realm of things. And so some of my friends joke with me, they’re like Oh, now you have a normal memory but it’s not trust me, it’s not. It’s definitely like a struggle but it’s something I can deal with and like have work to, like live with and, you know, only make it better. that’s kind of how it was for since it happened and whatnot.
Diagnosis and Watch-and-Wait
But I had the surgery that 2012 or January 2012 and they determined it was a grade two oligodendroglioma which is one of the major types of a brain tumor. So at the time because it was a low grade I had a good surgery. We decided to do a watch and wait period instead of going directly to chemo radiation just to kind of see how it go on. So after the surgery I didn’t have to do anything once I was kind of like getting myself back to feeling better. We ended up for my parents came home, back up to Portland and I had to as well because as much as I wanted to stay there and teach and live my life, it just wasn’t going to happen. Unfortunately, just because of everything I was going through and I needed support around me. So I moved back up here and was just going through whatever I could to work on my memory system and just kind of recovery from that and till it did grow back in. It was at the very end of 2016, early 2015. I didn’t necessarily feel the regrowth happening, but I was having so many deficits in general just from the surgery and the tumor itself to begin with that. And luckily, you know, I do get MRI’s pretty often so they were able to see something going on at the time. At the time I did have migraines, but it wasn’t as bad as it ended up becoming.
Rebuilding Life and Facing Regrowth
So I would say like in the to two years or so before the regrowth happened it was a lot of just focusing on getting better and then kind of learning to just become this new person kind of thing. I mean, there was things I would never be able to change. That’s just how it was. But there was also with memory it was, you know, just kind of teaching myself and learning words again. And I was lucky. If I look back now I didn’t have like the nausea that I do now. And there’s very, like things there’s a lot of things at least that I am grateful for, that I like in life. It’s kind of weird in the sense like before this all happened I kind of looked at life in like a view of I’m going to do this and that, and I have all these life goals and whatnot, and I feel like I now look at life differently, where little things around me mean so much. And just the simple things in life are like amazing to me, you know?
Deciding on Treatment: Chemo and Radiation
So once they discovered that there’s at the time they weren’t exactly sure if it was regrowth or just something popping up that they were curious about. So they kind of wanted to do multiple like MRI’s, like more put together than normal for about, I would say two months because it is like it was March when we finally decided like, okay, it’s treatment time. And that’s when we had the talk with the doctor about doing chemo and radiation together this time which is kind of like the known treatment when this kind of stuff happens because we’d already done a massive resection and it was kind of that time and again, it’s like I already had it in my mind that this was very possible. So I didn’t have that like surprised look or anything like that. I was again kind of like, okay this is the this is the plan. This is our going to do it. I’m going to get myself ready and I’m going to beat it like I always have. Like, that’s like the weird thing. People kind of ask me about is like, aren’t you like, nervous? Aren’t you worried? And obviously I am but at the same time I’ve never had the view of like this is going to like and me, as weird as that is because I mean I’ve already outlived like the average life expectancy and it’s I don’t know this is like kind of a crazy thing, but I haven’t really met anybody younger than me. That is like lived this long as hard as it is. And I almost at least tell myself that positivity has such a massive effect because at least for me just having that mindset and not even like thinking about death at least has done more than I have asked for.
Chemo-Radiation: The First Round
So after kind of getting it all put together it was going to start with the Temodar which is the chemo that I luckily wouldn’t have to do at the hospital. It was like pills for that I had and I would take that every night during the first section of doing chemo and radiation together. So I’d be taking the chemo every day and then I’d be doing radiation Monday through Friday for six weeks and that honestly, like for the most part, it started off well. It wasn’t probably till the like halfway through when I started getting like crazy tired did a lot of like bed rest for sure. So I started like a little blog to kind of keep everybody up to date on how I was, what things were like. And so and that was really fun. So once I did the six weeks of chemo and radiation I had a 21 day break where I wasn’t on anything and it was right around my birthday. My birthday’s in May. That was really nice.
High-Dose Chemo and a Scare
But then once I had to go back on my six month like round of a like way higher dose of chemo where it was only I want to say five days. The first or the first five days of each month. So it wasn’t like every single day. It was a higher dosage of it but only five days for six months. But I had to stop it after the fourth month in September. At the time times that was right after I had finished doing it I had a very bad reaction and they weren’t exactly sure like why this happened. It’s not common or anything like that. But it was it was really bad. I had my whole body break out into like a hives. Look, I couldn’t move my body. I ended up in the hospital and they at the time just said, okay, we have to stop it. There’s no way we can continue this. And I all like I was scared thinking like Oh no, like, is that going to work still? Like, do I need to finish it? Like, so I had that when I like in the back of my head just being like, worried and not exactly sure what to expect. But luckily on the good side it slowly went away after like not having got in my system anymore. So I think what they determined is my body kind of just said, no, we’re done. Like we can’t take it anymore which is it’s a bummer. But like at the same time I had a good like overall result at the end. So once that kind of came through it was like it was all worth it at that point.
Side Effects: Hair, Headaches, and Heartbreak
So that was again it was a mix of chemo and radiation. And so I’m not sure it was really giving me like the nausea, the aches, the pains. And that’s also when I started getting like horrible headaches, migraines. They have a feeling it’s not necessarily related to like that type of head pain but more like nerves and nerve damage that was going on because it was only on this side where everything was like going down. And I had a alone with the the sickness and the nausea and just the all of the stuff. I lost my hair in is very unique way because it wasn’t the chemo that did anything to me because I thought, you know most of the time it’s chemo that kind of has the hair loss. But I was lucky in that sense that the chemo that I was taking did nothing but the radiation on my head did. And I want to almost say it was in the perfect spot as weird as that sounds because the top part stayed on and the bottom part stayed on but in a very precise loop around the middle of my hair was gone. It was like a huge part of my life that was not expected. So when I was going to go through chemo and radiation I actually at the time when I found out that there was regrowth I was pregnant. I had just found out I was pregnant. But unfortunately I did have a miscarriage shortly after. And again, it might have been meant to be or just from like the stress I was going through, but that was really hard. And I think looking back, that’s kind of why I didn’t take the option of like saving my eggs. And I kind of just told myself back then that if it’s meant to be, it’s meant to be, but I’m just not in the place right now to, like, go through that and wanted to kind of you know, get the tumor done before anything.
An Unexpected Miracle: Becoming a Mom
So I kind of never really even expected to be able to have kids kind of thing. I knew I could, but it was very unlikely believe it or not, like a year after going through the chemo radiation I got pregnant and that literally, like blew my mind and was again like the happiest I’ve ever been, the greatest gift of my life. he my son his name is Brody is definitely like what keeps me going every every day, no matter what he’s what I fight for. So but after that I would do my MRI’s about I want to see it back then probably every three months for about maybe the first year. And once that got kind of cleared, like everything’s good, no regrowth every thing is like kind of like down rather than up, like the cancer cells at least. So everything was looking good. So for about six or seven years like in remission, which again I’m very thankful cause I mean, that’s that’s a long time in the whole like realm of range. There was no changes in my memory or deficits that had changed at this point in time. So I was doing well for the most part and kind of just going with the flow and enjoying what I could just go on with it.
A New Scare in 2021–2022
So December, right? So I have my MRI’s twice a year. So December 2021 on my first call because that was kind of during the COVID era. But so I had my doctor call me on the phone to go over my results of the MRI. And originally he was like You’re good. it’s always kind of short and sweet, like, you’re good don’t say anything. And that’s what happened at first. Then the next morning he calls me again and said he wasn’t exactly sure if it was like dead cells or tissue that was kind of popping up or like what exactly it was. But he did want to kind of like feel it sooner than later. So it was a very hard time, kind of just watching waiting and kind of like all right, like, what is this? Is it just like a scare or is it regrows? Like, what is going on here? And then once they did that second MRI is when they kind of said Yeah, it’s definitely something. We’re not exactly sure what we need to do a surgery again. And this was not a massive surgery like before. This was another type of small biopsy to kind of determine what’s going on. Has it changed? Has anything else happened? So that’s what we ended up doing about a month, month and a half later in April. Yes, it was in April 2022. That’s when I had my third brain surgery. That one actually went pretty well. It was short because there wasn’t much going on and so I was only at the hospital I want to say maybe like five days or less even. And I again the surgery went really well. And this time was different, though because I now had a son and somebody that, you know I, you know, is is my world and my number one I mean, even with my cancer and like everything I’ve been going through he will always be my number one no matter what.
Updated Diagnosis and Rare Findings
But once I got the results from the surgery is when it was like the biggest relief yet. Kind of like not a good thing because obviously I don’t want to hear there’s regrowth. Obviously, like that’s not a good thing. But on the good side of things, there hasn’t been any type of a higher grade that’s gone into it which is very rare, especially after going through radiation, chemo and just over the years especially in brain tumors they normally will grow into a higher grade over time. I always like in the back of my mind, knew that was something to be prepared for, but to hear that it’s still a low grade. So much relief was like going off and kind of made me like more relaxed even though it’s like not a good thing to go through at all. The one thing that like threw me for a loop was the fact that it was no longer considered a oligodendroglioma brain tumor, which that’s like what I’ve always looked into and learned about. So when they said, Nope you don’t have an oligodendroglioma anymore, you now have a grade two astrocytoma with a CH one mutation which probably makes no sense right now but that’s what I thought too. I’m like, okay, what is this? They still thought it was an oligodendroglioma but they did say it’s kind of rare that you don’t have the one p 19 Q co deletions which is more so a part of that. So now since all these changes they’ve made because I don’t have that I now considered a astrocytoma and the two main mutations that I have that have basically like caused a brain tumor is the Tp53 which is a gene or like a mutation that does a lot of or it causes a lot of cancers not just brain tumors, many others as well aside from tagging the news like, yes, you have tumors back it is still at a good level to deal with where normally in the past at this point I would probably have to go through my second round of radiation. And the weird thing with my chemo in the past is they still aren’t sure if I should ever try that type of chemo again just because of how it affected me.
Trying a New Chemo Path
But now with all of these other changes they’ve found a new type of chemo that’s actually used with a certain type of leukemia. Since my is at that level and still very slow with the growth they decided, you know what, we should try this because this might be something that is positive and could help you. There’s been a couple other people with my main oncologist one of my main doctors that’s had really good results with a few of his other patients and I was like, Yep I want to try. I will try anything and everything and even outside of the medical realm of things, I try to eat healthy and exercise seriously with coaching, cheer and being a mom. So doing all of that, I love yoga. That’s like my go to and just making sure things like around me 24 over seven are helping as well.
Living with Tibsovo: Daily Realities
So it’s going to be almost a year of going through all this is when I started the tibsovo that I take at night every night about 250 milligrams pills at night. And it’s been overall I would say, other than that. So the nausea was hard at first. I had to have my body get used to it. And so I would say after probably like four months or so I finally got to stop taking nausea medicine. And I still get the nausea here and there, but I’ve kind of like just learned to to live with it. And other than that just the head pain and the tiredness. That’s the other thing that hasn’t gone away is that I do get really like fatigue and it’s kind of hard to kind of put myself through things that were just so easy before. I will say it’s definitely stressful because it’s kind of like another watch and wait period of time because it’s not anything, you know like right here, right now. So I do have my MRI’s every other month and then I have my blood work done every month and my EKG is like I just kind of have to keep up and get all of that taken care of to just make sure things are going well. And so far so good. Usually by now it should have stopped the growth from what I heard and it hasn’t quite done that yet. It’s definitely slowed the growth for me, but it hasn’t like completely stopped it. So I’m like, great my next MRI will have a good outlook on that but there’s always a chance that if it does I might have to like start something else but I’m not going to like worry about that just yet and keep going.
Choosing Positivity and Purpose
Living with this for so long, especially this type of cancer and having so many good times with bad times as well. But I feel like having that positive mindset has done so much. Helping others is a huge thing for me for sure even if stuff like this does happen instead of kind of like putting myself down I try to think of the positives and like I’m not saying it’s easy. I’m not saying I enjoy having to do all this. It definitely has given me like the strength and just the fight again
Would you like me to convert this into a properly formatted blog post in your preferred Brand Voice later, or keep it exactly as-is with just headings and title (like above) for publishing?