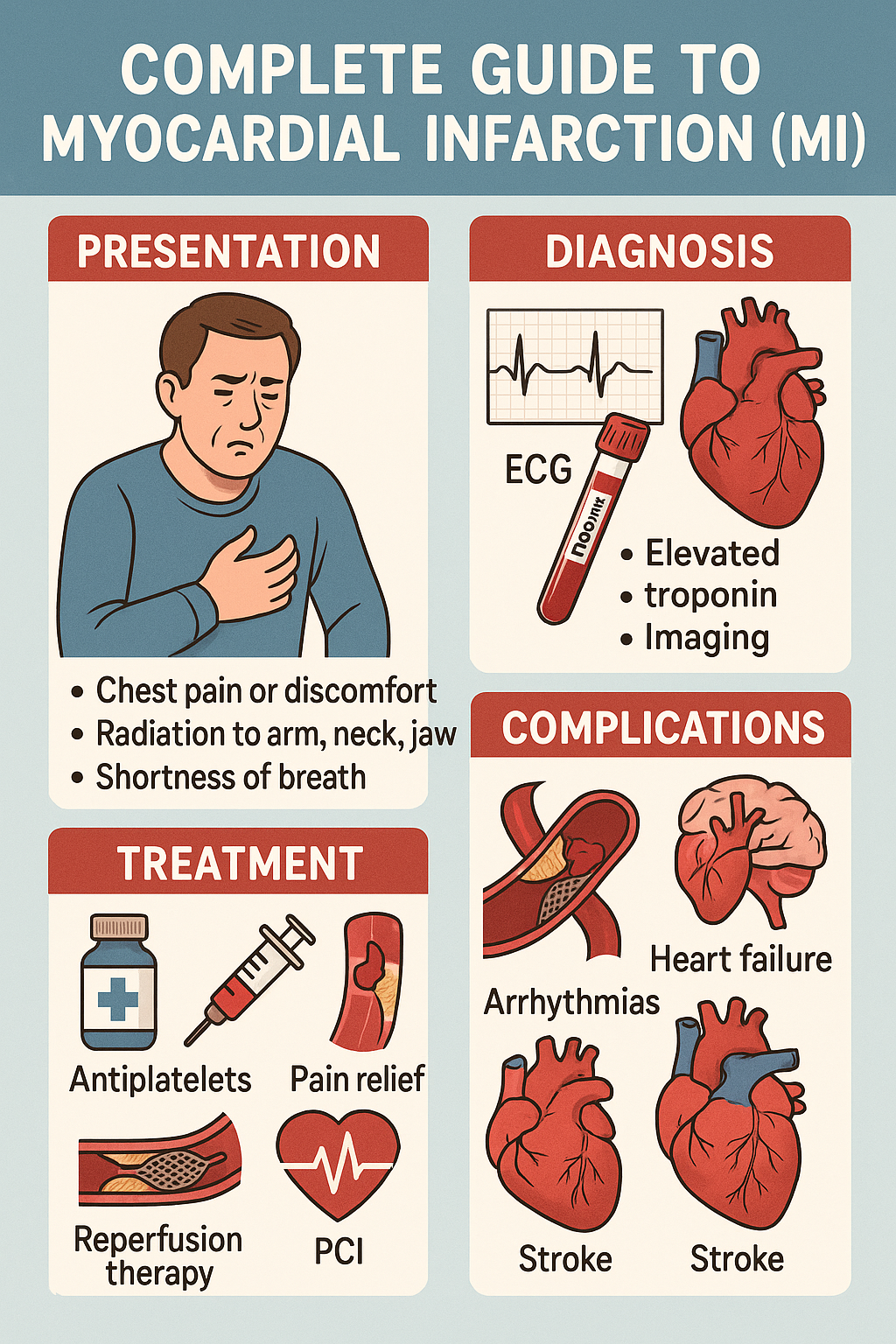
if a patient presents to you with a fist over the left side of the chest with an anxious look and sweating all over the face the first and foremost thing which should come into your mind should be cardiac pathology and mainly this is a angina and general pain the causes could be ischemia or infection and in layman terms the myocardial infarction is called as heart attack so in this video we will discuss what are the types of mri what is the pathology or why it is caused the etiology and the risk factors also we’ll discuss about the diagnosis how do we diagnose mi and the main part is the treatment of mi also we’ll be discussing about the complication and the last is the differential diagnosis so we’ll talk everything about mi in this video so keep watching this video till the end till that time i’ll introduce myself i am dr chirag madan working as an intensivist isu consultant at apollo hospital new delhi so without wasting much time let’s begin now talking about the clinical presentation as we discussed patients usually present with a fist over the left side of the chest which is called as levine sign important for your mcqs and this pain is usually intense substernal and usually remains for 20 to 30 minutes and maybe more and this pain could radiate to the jaw and to the neck also to the left side or left arm now the nature of the pain could be squeezing aching or burning sensation and some patient present with discomfort or pain in the epigastric area or sensation of fullness the other symptom could be fatigue or malaise and if we talk about the signs there could be increased heart rate which is tachycardia increase in blood pressure which is because of the sympathetic drive and there could be increased respiratory rate and in cases let’s say we’ll talk about later if there is inferior wall mi or a right ventricle infection then patient having a distended neck veins so this is uh these are the signs and symptoms which the patient presents with
What Is MI? Definitions and ACS Spectrum
now talking about the mi as the name says mi is myocardial infarction myo means muscle cardiac is obviously the uh the cardiac origin and infarction is death of the tissue or the necrosis right now we’ll uh discuss there are three different entities st elevation mi non st elevation mi and unstable angina and these three all these three entities they come under acs that is acute coronary syndrome right now as the name says coronary first of all the heart the function of the heart is just like a pump it pumps blood to the entire body and receives blood obviously from the entire body which is called as free load uh now heart itself get the supply from the coronary arteries if there is any pathology in the coronaries that causes acs and there we have all the three stemi and semi and unstable angina now how do you differentiate these three first of all and now we are coming on to the pathology so mainly these mi or these anginal pains are attributed by the atherosclerosis in the coronary arteries now this atherosclerosis along with a calf there is a fibrinous cap this is called as plaque now if the this is present in the coronary artery there is for sure impairment of the blood flow to the distal part which causes ischemia and this ischemia is responsible for the anginal pain so if a patient has just the ischemic there is no death of the tissue no death of the myocardial or the heart tissue then there is then it is just called as unstable angina so in unstable angina there is pain and if we talk about cardiac markers they are negative i’ll talk about in the later part of the video now let’s say this plaque is somewhat uh partially occluding the coronary artery right somewhat occluding so there is further impairment of the blood flow to the distal part which obviously causes ischemia and there is some infection also infection is death of the tissue now the death of the tissue causes or the necrosis of the tissue causes release of troponins in the blood which are called as cardiac biomarkers or cardiac enzymes right and this is a contractile protein by the way the troponins so uh these are released whenever there is infection of the heart tissue or the myocardium so the in in this second entity there is sub endocardial infarction or necrosis right sub endocardial this is not not full length just the sub endocardial and in usually in these kind of situation there occurs depression of the st segment or inversion of the t waves so this entity is called as n-stemi that is non-st elevation mi whereas if we talk about the third one and the third entity is stemi where there is full occlusion of the coronary arteries now uh there is a plaque if plaque ruptures or fissures right so that causes accumulation of the platelet at the site and that causes full occlusion of the coronary arteries now when it is fully occluded obviously the there is no flow of the blood to the distal part and then the whole muscle is infected or dead now this total is called as transmural involving all the layers so trans neural infection is there in stemi and all because whole of the tissue is now gone or infected there is intense release of cardiac biomarker mainly troponins so now again revising all the three in unstable angina there is just the pain there is there can be changes but cardiac markers are negative there are no troponins in the blood talking about the n-stemi the there is for sure and general pain if we see the ecg there is either uh no st elevation mi or you can say there can be st depression with or without t wave inversion and having a cardiac biomarkers in the blood that means troponins are present right on a higher side talking about the third one that is the stemi in this obviously there is angina pain then in the ecg there is st elevation and thirdly there is for sure increase in proponents in the blood level so these are the three different entities along with the pathology which we discussed
Risk Factors and Causes
now we have discussed why it happened the cause mainly there’s atherosclerosis the plaque formation and the rupturing now in which individual this is on a higher side or what are the risk factors so they are firstly non-modifiable risk factor which are age the sex of the patient the genetics of the patient right these are non-modifiable and if we talk about modifiable risk factors the first and foremost i’ll talk about is smoking that irritates and causes plaque fishing or rupture of the blood second it could be the increased blood pressure third it could be increased in cholesterol or the lipid content fourth obesity fifth stress to the patient so these are the causes which increases the risk of having a mi or the angina pain also myocardial infarction has five types type one spontaneous mi in which there is plaque rupturing plaque fissuring erosion of the plaque right second is due to imbalance between the oxygen demand and supply which happens in coronary embolus coronary artery spasm and type 3 is mi resulting in cardiac arrest when biomarkers are unavailable or you are not able to send the biomarkers even right now type 4 is divided into 2 4a and 4b 4a is related to pci percutaneous intervention 4b is related to strength thrombosis and type 5 is related to cabg so these are the five types of mi which you should be knowing
Diagnosis: Tests and ECG Basics
now talking about the diagnosis so whenever you are having this kind of presentation so you are thinking in terms of cardiac pathology the blood samples you need to send is first of all you have to check the blood sugar whenever the patient is having this kind of discomfort anxious and sweating blood sugar is to be done first and foremost second is complete blood count third is cardiac biomarkers mainly the troponin eye and nowadays which what we are using is high sensitive troponin eye right it is the earliest marker to be detected in the serum and you have to see the serial uh serial values at zero are zero i mean at the presentation in three hours then six hours then fourth is the lipid profile of the patient and then obviously you send the other blood investigation like kidney function test and liver function test also apart from that to make a diagnosis you need a 12 lead ecg also very very very important and i’m so much excited and happy to say that we have recently released our ebook on ecg and i’m extremely happy with the response which the ebook has got i mean i didn’t expected this kind of response so thank you so much guys thank you so much for the love and support you have shown to our ebook in that we have discussed uh 10 basic steps how to read or interpret an ecg in a simple and interesting manner and also there are questionnaires at the back of the ebook and along with that you will get a free live lecture with the ecg ebook right and you can find the link in the description box below so now coming back to the topic as you can see over here uh these are the limb leads and 2 3 avf are in the lower part or the inferior part so if 2 3 avf has st elevation or j point elevation then this is called as inferior volami because inferior wall is involved now if there is st elevation or j point elevation in one or avl that goes in favor of lateral wall so one avl also v5 v6 that goes in lateral volume if v1 and v2 are involved then septal if v2 to v4 is involved then anterior wall and if from let’s say v1 to v4 it is called an antroceptal also using these areas you get to know which coronary artery is mainly involved if it is in fear of all mi so mainly it is rca right coronary artery right uh so i’ll not go much in detail uh in this video so this is just about the diagnosis how do we diagnose it now apart from ecg you can go for cardiac imaging meanly echo echo cardiography now this tells you regional wall motion abnormality which we normally call as rwma so this was about the diagnosis
Initial Management and Definitive Treatment
now the main part is the treatment so whenever you have these kind of patient in pre-hospital setup i mean the patient is just in the ambulance or at home the important thing is to give a loading dose of anti-platelet mainly the aspherin which is normally a loading dose of 300 milligram but uh out this is in india outside india they they prefer to have in multiples of 81 so 81 162 325 right so uh so so you can find that in books also in india we give a loading dose of 300 milligram of aspirin right and there is a mnemonic called as moon m-o-a-n so a stands for aspirin now the other thing is o is oxygen supplementation it is to be given whenever the saturation is less than 90 percent or peo2 is less than 60 milliliters of mercury otherwise there is no use in fact in uh it has been somewhat found to be detrimental right so always supplement the oxygen whenever the patient is hypoxamic saturation less than 90 or po2 less than 60 right the third is n is nitrates so this nitrate is very very helpful to the patient so you can give as a sublingual tablet point four milligram whenever in pre-hospital setup and this normally causes decrease in vascular resistance svr and causes decrease in preload also right and this also dilates visor validate the coronary artery causing relief of the pain right so nitrates are to be given to the patient and whenever the patient is in hospital setup try to give iv ntg at a dose of 5 to 10 micrograms per minute right and but whenever the before giving nitrate you need to check the blood pressure of the patient if the patient is bradycardic or hypo hypotensive do not give nitrates secondly uh to get a relief from the pain you can give iv morphine also two to four milligram so this is just whenever you see the patient in the emergency or in the pre-hospital but the best or the definitive treatment is the reperfusion which is called as pci percutaneous coronary intervention in this you do first of all angiography using a dye you see which artery is occluded or not and if at all the artery is found to be occluded then you can open it using a stenting so this is called as angioplasty angiography and angioplasty right so this is the definitive treatment and it has to be done with the dough to needle time of 90 minutes so the door is the hospital rule right so door to needle should be 90 minutes as early as possible and to be done uh whenever the symptoms is less than 12 hours whenever you are planning to have a pci done before that you need to load with another anti plated also which is p2y12 receptor antagonist there are three of it first clopidogrel second t-controller and third procedural the loading dose of clopate is 300 to 600 milligram so normally we give 300 milligram of clopidogrel secondly is uh ticagrelor the loading dose of 180 milligram and pressure the loading dose of 60 milligram right and if at all let’s say patient is not undergoing pcr then also you have to give clopidogrel or any of these three along with aspirin also right now let’s say there is no facility of pci in a hospital or the the clinician is not able to perform this they are not capable to do the pci uh then the other alternative is fibrinolysis previously there was a streptokinase was used but now it is not used because of the complication rates now the agents which are used are tenecteplase alti place and retiplase the 1080 place is normally used with a dose of 30 milligram in less than 50 kg and 50 milligram and more than 90 kgs so the dose is 30 to 50 milligram right now after initial management you have to do a maintenance therapy which is by lifestyle modification adding beta blocker or arvs and third is continuation of dual antiplatelet for it in a maintenance dose for at least one year right so this is the maintenance
Complications
now complications of mi so you can remember the complication by an mnemonic mad pals where m stands for mechanical rupture which could be left ventricular free wall rupture interventional rupture or papillary muscle wall rupture right a stands for arrhythmias d stands for dressler syndrome which is post myocardial infarction syndrome and normally it is a autoimmune phenomena and which is which usually develops after two to three weeks of mi and presents as a pericarditis or plural effusion a pericardial diffusion then p stands for pericarditis a stands for uh aneurysm of left ventricle l stands for lvf or you can say as pulmonary edema and s stands for shock which is mainly cardiogenic shock so this is just a mnemonic so as to memorize it
Differential Diagnosis
now talking about the differential diagnosis because whenever you have this kind of presentation don’t get biased to cardiac pathology only you need to have a differential also so it could be grd or acute gastritis or they could be aortic dissection acute cholecystitis then there could be mitral regurgitation or aortic regurgitation simple anxiety disorder right or there could be pericarditis myocarditis or even pulmonary embolism right pneumothorax and pneumonia even so you need to rule out everything so this was all about mi or if you talk about the ischemic heart disease i hope you liked the content of this video if yes please hit the like button and share with your friends and colleagues and do not forget to subscribe this channel to get the latest updates of our new videos thank you so much guys bye bye take care
Would you like me to style the headings as H2/H3 or keep them as plain bold in your editor?
Leave a Reply